According to the World Health Organization (WHO), a very high percentage of
80-60 year olds suffer from some degree of joint cartilage erosion. However,
joint erosion is not the exclusive domain of adults, and it may occur even in
younger people.
Robotic arm-assisted hip replacement is the last resort for joint pain. It is
customary to resort to this option only after the conservative treatment
methods have been exhausted, including physiotherapy to improve movement
ranges and strengthen muscles and various injections for the treatment of
inflammation.
Structure of the Hip Joint
The hip joint is the second largest in the body after the knee joint; it connects the pelvis to the lower limbs and carries a lot of load. Its shape is similar to that of a pestle and mortar; the rounded femur head fits the pelvic socket (acetabulum) precisely, and the thigh head and acetabulum are wrapped in a layer of cartilage whose function is to stop and absorb shocks and allow the smooth movement of the hip joint.
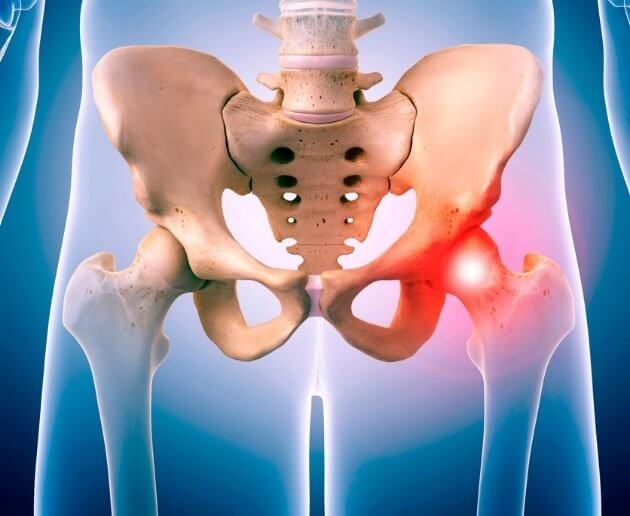
The hip is encased in the Capsula Articularis, which consists of thick
connective tissue that provides it with support and stability while allowing
movement in several directions. There are large muscles surrounding the hip
joint – the gluteus muscles that enable movement and stabilize the pelvis.
What are the signs of erosion of the cartilage from the hip joint?
Cartilage is living tissue that receives a blood supply and innervation from the bone below it (subdural bone) and from the joint fluid (synovial fluid). Erosion of the joint cartilage leads to an inflammatory process and to the exposure of the subchondrial bone in which there are nerves. As a result, pain develops, and movement of the hip joint is restricted. Pain can be relieved with painkillers, anti-inflammatory treatments, various injections, and physiotherapy.
What are the causes of wear and tear of the hip joint?
- ∙Damage to the hip joint – direct or indirect.
- ∙Excess weight and advanced age that may cause erosion of the joint
cartilage. - ∙Factors whose incidence varies with age:
- In childhood: developmental or congenital diseases of the joint:
DDH – Developmental Dysplasia of the Hip, and Perthes. - In young adults: congenital or developmental problems, sports
injuries that damage cartilage and the labrum, as well as AVN –
avascular necrosis of the head of the femur (Avascular Necrosis)
resulting from impaired blood supply to the head of the joint. - In the older population, the most common cause of cartilage
damage is degenerative erosion of the cartilage – Osteoarthritis. - Trauma to the joint: fracture or direct injury.
- In childhood: developmental or congenital diseases of the joint:
Conservative treatments for hip erosion
There are cases where it can be determined that there is no need to perform hip replacement surgery as yet. In these circumstances, the attending physician will offer a number of alternative treatments aimed at relieving pain and inflammation by improving the movement abilities of the joint through physiotherapy exercises to strengthen the pelvic muscles and improve the range of motion of the hip joint. In addition, drug treatments given orally such as painkillers, anti-inflammatory drugs or supplements containing mainly glucosamine and/or chondratine may be tried out, and injections may be administered into the affected joint directly. These are steroids that act on the inflammation, hyaluronic acid to improve joint function, stem cells, PRP – platelet-rich plasma, etc.
When should you seek hip surgery?
If conservative treatment has not brought any improvement, the pain has become permanent and you suffer from a significant functional limitation – you may be a candidate for hip replacement surgery – contact us for initial consultation and an examination.
What is special about Professor Drexler's method of robotically replacing a hip joint?
Hip replacement surgeries are considered the most successful in the field of orthopedics, and within a relatively short period of time enable a significant improvement to the quality of life of the patient and a quick return to routine.
This is a special robotic arm controlled by the surgeon and makes it possible to plan the operation well in 3D systems, predicting the entire range of motion of the joint and making highly accurate bone incisions, while balancing the joint anatomically and maintaining equal leg length. Robot-assisted surgery makes it possible to position the implant in a way that simulates the anatomical actions of the natural joint, which creates a better and anatomical distribution of loads.
Due to the precision and maintenance of defined cutting limits, the damage to muscles and tissue surrounding the joint is very low. All of these things contribute to rapid recovery, effective rehabilitation, and a reduction to the patient’s pain level. Not only that, in the event of a deviation, the robotic arm will cease its activity and prevent damage to the surrounding anatomy and tissues.
Professor Drexler’s method has other advantages:
Partial Anesthesia – Spinal anesthesia and not general anesthesia (as far as possible) – For most of the population, spinal anesthesia (half of the body) is sufficient, without the need for full anesthesia. The anesthetics are injected into the lower back, into the casing of the spinal cord with a thin needle; they work for four to six hours, during which the patient will not be able to move his leg and can be operated on without pain. Partial anesthesia reduces the side effects associated with full general anesthesia such as nausea, vomiting, dizziness and so on.
Short hospitalization – Duration of hospitalization is one night and the duration of surgery is about an hour (after a preparation process and anesthesia lasting another hour).
Shortening the rehabilitation time and quick return to routine – a few hours after surgery, Professor Drexler is already setting up and accompanying the patient in his first steps, with and without a treadmill, with an emphasis on the correct gait and transferral of the load to the legs in order to avoid limping that would cause back pain and weakness of the pelvic muscles.
Healing at home – The patient is discharged to his home the following day when he is able to walk and operate the hip. There is no need for institutional rehabilitation, and a physiotherapist will come to the patient’s home to practice hip flexion and strengthen muscles. Healing at home allows the patient to be surrounded by his family and friends and encourages him to walk freely and move the hip without being dependent on others.
Stages of hip replacement surgery with a robotic arm:
In the first stage, Professor Drexler creates access to the joint by cutting the side of the thigh. The acetabulum is cleaned of tissue residue with a special drill, and the cartilage is removed; then preparation is carried out for the formal canal using a planing device.
Professor Drexler, who is one of the pioneers in using a robotic arm for joint surgery, will place the implant in an anatomically accurate manner with the help of the robotic arm, while continuously monitoring of the angle and placement of the implant according to the surgical plan, in order to ensure the expected result.
Possible complications of robot-assisted hip replacement surgery
Every surgical operation involves risks and complications, including nerve damage, damage to blood vessels, infection and complications of anesthesia, however in surgery to replace a hip joint performed by a robot and under partial anesthesia the probability of complications is very low and stands at between 1% and 2%.
Apart from the systemic complications, there may be complications specific to the area operated on. These include a fracture of the femur or acetabulum, dislocation, damage to the sciatic, gluteal, femoral nerves, or the LFCN (depending on the surgical approach), leg-length differences, and stiffness of the hip joint (which usually passes over time).
It is important to note that the medical staff explainsthe possible complications and risks involved in surgery at length prior to surgery. During the preparatory stage, Prof. Drexler and the anesthesiologist meet with the atient and present the risks and potential complications according to his individual condition.
The Recovery Process
It is of great importance to activate the hip joint in the immediate range in order to prevent stiffness and atrophy, so six hours after the operation Professor Drexler gets the patient up, and he takes first steps with him and accompanies him in the practice of going up and down stairs. In addition, the patient receives a prescription for pain relief medication, and later the patient will practice physiotherapy exercises at home and will walk, first on a treadmill, and then with a walking stick. In addition, the patient will have to practice exercises at home on a regular basis for several weeks in order to strengthen the joint and increase the range of motion.
Robot-Assisted Hip Replacement Surgery Results
It is very important to coordinate expectations between the surgeon and the patient. Even though the surgery has a very high success rate, it is not usually possible to guarantee a 100% success rate. However, it is certainly possible to achieve the main goal of the surgery, and bring about improvement to the quality of life in such a way that the hip will cease to be the center of life due to the limitation and pain.
See the success stories of patients who underwent mini posterior hip replacement surgery under Prof. Drexler:
Selection of the attending physician
A successful medical process is the product of choosing a medical practitioner who is proficient in the field of treatment and has the appropriate equipment and knowledge to perform the operation.
Prof. Michael Drexler currently serves as the Director of the Orthopedic Department and the Joint Replacement Unit at Assuta Hospital in Ashdod. In addition to his work at Assuta, Prof. Drexler is a clinical associate professor in the Department of Orthopedics at Ben Gurion University. At the beginning of his career in the field, Prof. Drexler performed knee replacement surgery around the world, while training the best surgeons, and completed advanced training and surgery in Canada, Germany and New York. His experience and reputation make him one of the leading experts in the field of joint replacements, especially that of knee and hip replacement.

Prof. Drexler is one of the pioneers in using a robotic arm for joint surgery, and has the most experience in the field.
Professor Drexler is a surgeon at Assuta Ashdod, Assuta Ramat Hahayal, and Rafael Hospital. To schedule a professional consultation to determine the appropriate treatment, and to schedule an appointment for hip replacement surgery, contact Professor Drexler’s clinic today at the Center for Advanced Orthopedics at Assuta Hospital by calling 050-4378437.